If you haven’t noticed yet, I read a lot about food and nutrition. 20 years ago it was cookbooks and cooking magazines, but about 10 years ago it shifted to books focused on the nutritional aspects of food and various diets. I wasn’t drawn to any of them on a quest to lose weight; it was more out of curiosity, and a desire to understand whether there were links between the things I (and my family) were consuming and a couple of chronic health issues we were experiencing.
Along the way, I started paying attention – really close attention – to how my body reacted after I ate certain things. Sometimes a reaction was immediate (I’ll spare you the details of what happens to me when I attempt a milkshake); sometimes it was considerably more delayed (big flare-ups of the nagging inflammatory arthritis in my left elbow a day or two after too much sugar – often in the form of . . . ahem, and boohoo . . . wine).
“Strepisodes”
At one point in the early 2000s I was diagnosed with Hashimoto’s Thyroiditis when my PCP was feeling around my neck and throat after a 5th or 6th bout with strep in the course of just over a year. (I had gotten to the point where I could count on the sandpapery-throat feeling that accompanied its onset at least once a quarter. I called them “strepisodes.”) He discovered that my thyroid was enlarged, sent me off for bloodwork and bang – the Hashimoto’s diagnosis. I’d never heard of it, and had no outward symptoms, but we (some me, a lot my husband, who gets like a bulldog with research) started reading more about it. In his more in-depth exploration, my husband discovered a link between excess fluoride consumption and thyroid problems, which would otherwise have been a finding that would have elicited a shoulder shrug. BUT, we had discovered not long before that time that our well water was naturally, and exceedingly, high in fluoride. Like, thousands of times higher than recommended levels. So I stopped drinking it. We installed a reverse-osmosis filter under our kitchen sink and a 2.5 gallon bottle of water took up permanent residence on the top shelf of the refrigerator.
Additionally, with each of the “strepisodes” I’d experienced up to the time of my Hashimoto’s diagnosis, I was given “Z-Packs” of azithromycin antibiotics. This PCP was new to the practice, so he hadn’t been a party to those earlier treatment decisions, but he concluded that the strep I had was systemic, and opted for a scorched earth course of treatment to knock it out once and for all, before it did real damage. He put me on a much stronger, and much higher-dose course of antibiotic (wish I could remember which one), which consisted of 3 “horse-pills,” 3 times a day, for 2 full weeks. I haven’t had a “strepisode” since, and I think I’ve been on antibiotics 3 times in total in the intervening 16 – 18 years.
I also started practicing yoga shortly after that diagnosis, not because of it, but for reasons I can’t quite articulate (a whole other story, which I shared in a non-Food Friday post several weeks ago). My lifestyle began shifting rather dramatically as a result, and when I went back to the doctor for my physical the next year (to another new PCP in the practice), having dutifully done my bloodwork the week before, she was surprised that all evidence of Hashimoto’s was absent. She said she’d never seen a case of Hashimoto’s being reversed. She asked me what I’d done. I told her I stopped drinking my super-heavily fluoridated water, and started doing yoga. It wasn’t until many years later, when I became intrigued with, and began learning more about the microbiome, that I recalled that third variable: the cessation of routine rounds of antibiotics.
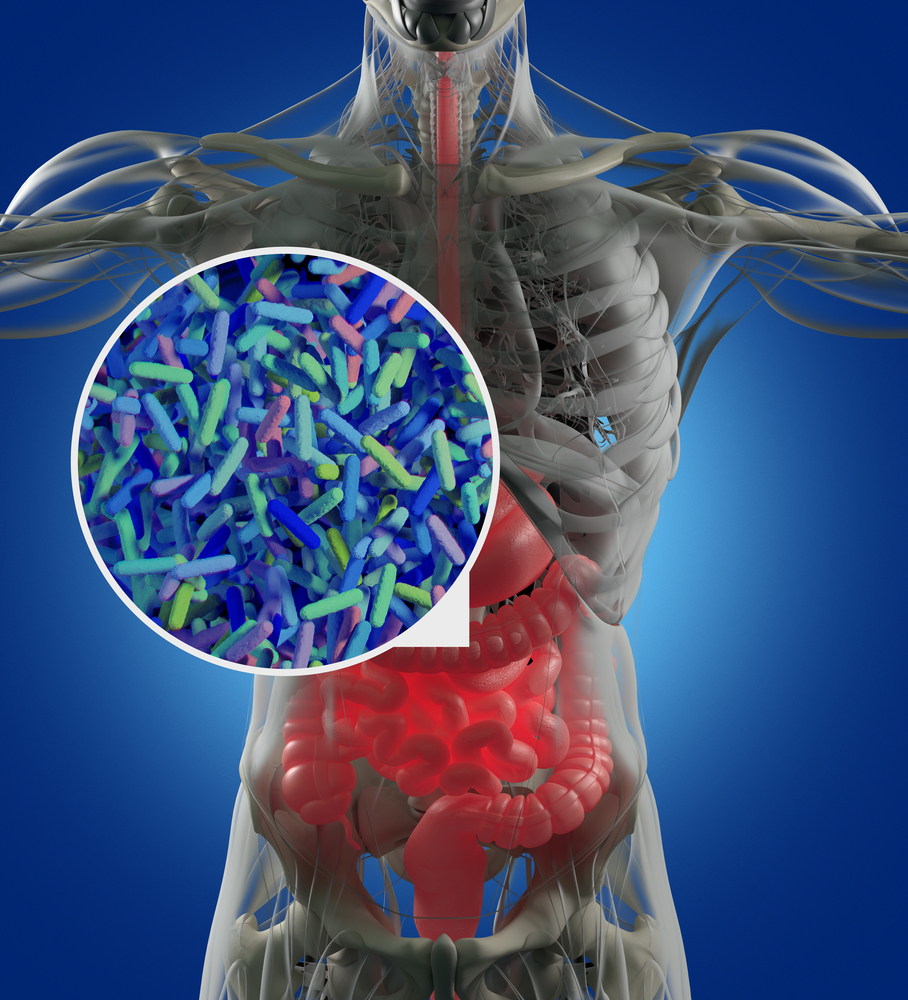
Enter the Microbiome
The microbiome fascinates me. If you aren’t familiar with the term, it refers to the natural bacteria that live, by necessity, inside of us (sorry germaphobes – that’s just how it is). In most healthy people, the “good” or beneficial bacteria outnumber the bad/harmful ones. We aren’t born with a microbiome – we acquire it, first through natural birth (or not, if natural birth doesn’t occur, e.g., birth by caesarean section); second, and continuing throughout our lives, through exposure – what we consume – consciously or unconsciously. That’s the boring part (though it’s far from static and can, and does, absolutely change as we change what we consume).
The fascination begins for me here: about 70% of the immune system lies in the gut. If you have an autoimmune disease and you aren’t actively aware of the potential impact of your microbiome on your condition, it could be worthwhile to learn more about it. Equally important (and utterly absorbing to me, if you’ll forgive the pun) is the interaction of the brain and the microbiome, one of the major components of which is the vagus nerve. Lots of things fell together for me once I learned about all of this: 1) how it’s possible for my body to react as quickly as it does when I attempt to enjoy that milkshake; 2) why I often experience a similar bodily response when I’m extra-anxious or nervous; 3) why it’s so important to eat slowly and chew your food thoroughly – something I’ve heard for years and kind of accepted, and now understand why: it’s the chewing that kicks off and sends the signals to your gut about what enzymes to release to properly deal with what’s in your mouth, and if you don’t chew enough, there isn’t enough time for the body to recognize what you’re eating; 4) maybe the reason my Hashimoto’s appeared was that the recurring use of the Z-packs was killing my microbiome! As I mentioned above, I absolutely experience flare-ups of the inflammatory arthritis (an autoimmune condition) in my left elbow when I eat too much sugar (or drink too much alcohol). It all made sense.
That’s a no-go(gurt); and Flunkin-Dunkin
What you eat and drink serves to promote certain types of gut flora, both “good” and “bad.” Sugars of all kinds appear to hinder the balance of beneficial organisms. Though it’s unclear how direct that link is in humans (not enough studies yet), there’s enough evidence in studies of mice that, if you ask me, we should be aware and paying close attention to our sugar intake. Similarly, artificial sweeteners may not be a good alternative, either. And when I’m talking about sugar intake, I mean not just what you get from cake or candy or other, obviously sweet things, but also the byproducts of refined carbohydrates (white bread, etc.). So, if you’re thinking that “Gogurt” spiked with processed fruit and loaded with sweetener is going to help your kid’s microbiome, it’s pretty much guaranteed to not be as good as a cup of plain yogurt with fresh fruit.
It took me some time to “retrain” my tastebuds away from sweet things, but now that I have, it’s amazing how crazy-sweet I find the contents of most boxes, bottles, and containers of things on the shelves at the supermarket. I even gave up my previously favorite guilty-pleasure: a Starbucks mocha. Yikes. Just the thought of one of those now makes my teeth hurt, and I absolutely *cringe* at the idea of what might be in garbage like those Dunkin COOLATTAS® or “signature lattes.” I genuinely believe this kind of junk is slowly killing us.
Supplement Snag
There’s a mountain of information out there about the microbiome now, and sure to be more as attention and interest increase in the public and in scientific research, but a word of caution: often the information you’ll find is part of the sites of people trying to sell you supplements, and there’s pretty much zero evidence that probiotic supplements are beneficial, other than for people with very specific conditions, such as Irritable Bowel Syndrome. As is the case with supplements in general, the body is much better at synthesizing what it needs from real food than from extracted or manufactured vitamins, minerals, etc. Even one of my favorite books on the subject is authored by a doctor who has studied and experimented with diets to alter/improve the microbiome, and while he says supplements are not necessary, he claims that *his* supplements can improve the effects of a microbiome-supporting diet. What a load of crap.
In an upcoming post, I’ll talk about what I’ve learned *can* help develop a healthier microbiome and point you to more sources you might find useful if you’re interested. The good news: none of this is difficult to achieve once you understand more about the types of foods that benefit the microbiome, and most of them are not exotic or hard to find.
Until then, happy Food Friday!!



2 Comments
Fascinating post!
Thank you Elizabeth!! It’s definitely a fascinating area!